Haglund Deformity Correction
Contents
Anatomy and Function
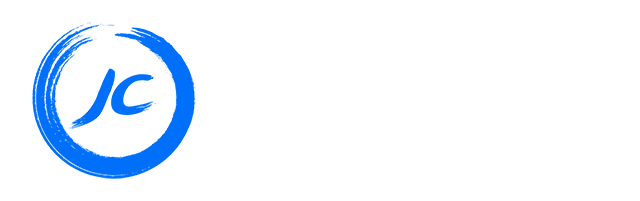
The Achilles tendon connects the gastrocnemius and soleus muscles (calf muscles) to the calcaneus (heel bone). It is the thickest tendon in the human body. It arises from the soleus-gastrocnemius complex of the calf muscles and inserts on the calcaneal tuberosity of the calcaneus. The insertion point on the calcaneus is surrounded by sacs or “bursa” which serve to act as cushioning. The tendon allows for contraction of the calf muscles to cause plantarflexion of the foot (standing on tip-toe).
Haglund’s Deformity and Pathophysiology
Haglund’s deformity was first described by Patrick Haglund, a Swedish doctor, in 1927. It is described as abnormal bony enlargement at the site of attachment of the Achilles tendon on the calcaneus. While it is a common clinical condition, its aetiology (cause) is still poorly understood. This bony lump can cause irritation of surrounding soft tissue and bursa especially in patients who wear tight or rigid shoes. This can progress to inflammation of the bursa (retrocalcaneal bursitis, Achilles bursitis) as well as of the Achilles tendon. When this inflammation occurs in the context of a present Haglund’s deformity it is described as “Haglund’s syndrome”.
Presentation and Symptoms
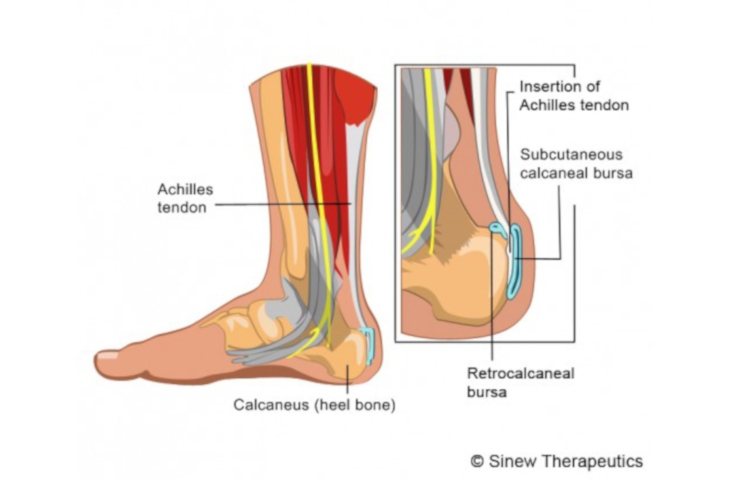
Most patients present with heel pain which can be associated with limping or swelling. The pain is most prominent while walking or other weight-bearing activities. On examination of the heel, a bump can often be appreciated as seen below. Signs of inflammation such as swelling, warmth, redness, and tenderness over the heel may also be present. An XRAY may demonstrate a bony prominence of calcaneus, as well as associated bone spurs at the Achilles tendon insertion. An MRI can demonstrate bony bodies adjacent to the calcaneal insertion of the Achilles tendon and can also evaluate for any underlying Achilles tendinopathy.


Treatment Options
There are various conservative treatment options:
Shoe modification: wearing backless or soft-backed shoes can reduce irritation
Cold therapy: applying ice to the affected area for 10-20 minutes can reduce swelling
Orthotic devices: heel lifts, pads, and arch supports can decrease pressure on the heel
Physical therapy: stretching exercises can relieve tension from the Achilles tendon
Medication: Oral non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can reduce pain and inflammation
Surgery
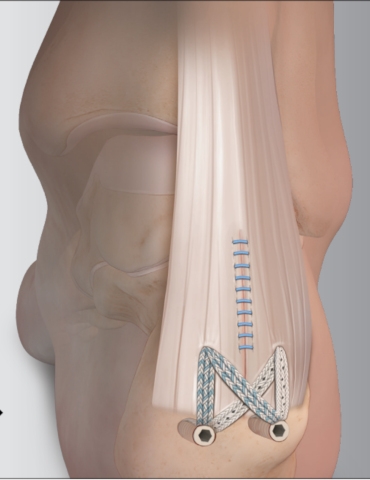
If conservative management has failed surgical intervention may be indicated. There are various techniques that can be used. One such procedure frees the Achilles tendon from its insertion on the calcaneus after which the abnormal bone is removed. The Achilles tendon is then reattached to its anatomical insertion on the calcaneus using a suture construct with suture anchors.
Postoperative Care and Rehabilitation
The patient is placed in a splint and is non-weight bearing for the first 2 weeks or until their first postoperative appointment (whichever comes first). At the first postoperative appointment the splint and sutures are removed, and the leg is placed in a short leg cast. Non-weight bearing is continued for a further 2 weeks. At 4 weeks postoperative, the cast is removed and the ankle is placed in a cam walker boot and weight-bearing is progressed as tolerated. Physical therapy exercises are started at this point. Most patients return to full activities between by 6 months.